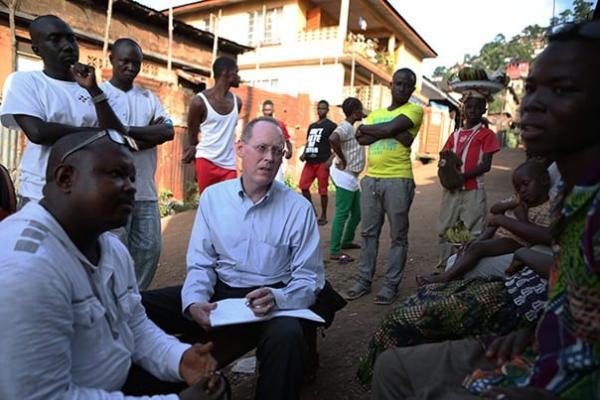
We need to provide better care for Ebola patients. That is the main point that physician-anthropologist Gene Richardson and co-authors, including Partners In Health Co-founder Dr. Paul Farmer, make in a recent comment in academic journal The Lancet Global Health. As obvious as the opinion might sound, it is contrarian, even rabble-rousing.
Richardson and his colleagues’ argument builds on a thought experiment. Imagine you are a West African in late 2014, the height of the Ebola epidemic. You’re feverish, vomiting, and headachy. Westerners are exhorting you to enter an Ebola treatment unit. What would you do?
You would probably do two things, the authors show. First, you would recognize that you might have nothing more than malaria, a largely non-fatal disease with the same symptoms as Ebola.
Then you would calculate your various odds of survival as best you could. (History provides us statistics to calculate the odds precisely.) To wit, if you have malaria, your chance of dying is .2 percent if you stay at home, and 16.1 percent if you get in one of those unsanitary ambulances and wait in a treatment unit’s messy triage area. If you have Ebola, your chance of dying is 70.8 percent at home and 64.3 percent at a treatment unit. Average your odds of survival according to where you go, instead of what mysterious disease you’re suffering from, and you have a 35.5 percent chance of dying if you stay at home, and a 40.2 percent chance of dying if you go for “treatment.”
In other words, a wise person in Sierra Leone, Guinea, or Liberia would ignore Western pleas. “You would be acting in your rational self-interest by staying at home,” the authors write, “not factoring in 1) rational desires to die at home rather than in (or in the queue in front of) a far-off tent; 2) rational fears that you might never see your family again; 3) rational responses to the pervasive messaging that Ebola has no cure” and so on.
The authors’ deconstruction of “rational” choices becomes controversial in context, however. Many in the global health community are not, and were not, eager to acknowledge the sagacity of people who avoided treatment units. A recent report by the World Health Organization provides an example. “All the modeling analyses show, as expected, that admitting patients to Ebola treatment centers and shortening the delay before hospitalization could have played a large part in slowing the increase and accelerating the decline in case incidence,” the report says.
Paragraph after paragraph focuses on corralling people and allowing the epidemic to burn itself out, while hardly mentioning the role of proper doctoring. It indulges in the “fetishisation of containment-through-isolation,” the Lancet authors write, instead of acknowledging the deadliness of treatment units.
And the line of thinking begets even worse ideas, the authors show. Rather than treating potential patients as people, global health experts see them as “superspreaders” or “vectors”—like creatures in a sci-fi movie. They label potential patients “‘unwilling to seek medical care,’” when such care is non-existent,” the Lancet authors write.
In just seven paragraphs, the authors extend their argument further—into history, anthropology, social theory, and more—but it all goes to underscore a single point: Don’t blame people, heal them. It’s good advice whether there’s an epidemic or not.