Tuberculosis (TB) is often thought of as an illness of the past, despite the fact that it’s the world’s deadliest infectious disease today—claiming a life roughly every 20 seconds. Countries around the world grapple with its devastation as a lack of resources places proven TB care and prevention out of reach of people who need them most.
Even the United States—which spends more on health care per person than almost every other wealthy country—is currently experiencing one of its largest recorded outbreaks of TB, centered in Kansas.
“While outbreaks are alarming, it’s actually a good thing that we are finding them,” Lindsay Palazuelos, PIH senior director of policy and program replication, said. “It’s good when we have the public health infrastructure to find outbreaks, and reminds us that we need to keep strong public health workforces and institutions so that we can drive down rates of TB in the U.S. as well.”
TB has always been a disease that hurts the impoverished the most. When you’re chronically malnourished or have other illnesses like HIV that impact your immune system, are unable to access health care, or are living in a densely populated area, you can be more susceptible to TB and experience poorer outcomes.
“Although tuberculosis is inextricably tied to poverty and inequality, experience shows that modest interventions have effected dramatic changes in outcome,” late PIH Co-founder Dr. Paul Farmer wrote in “Infections and Inequalities.” “Pragmatic solidarity means increased funding for tuberculosis control and treatment. It means making therapy available in a systematic and committed way.”
Many folks in the U.S. may not have heard of, or worried about, TB in their lifetimes. However, in the countries where PIH works, TB is all too well known. People may not have heard all the scientific details, but they understand TB’s impact because they’ve seen friends, neighbors, and loved ones who have fallen sick or died from the disease.
TB is, however, completely preventable and curable. So, why are over 1.2 million people dying of this disease every year? Let’s learn more about the disease, how it spreads, and how we can be a part of the movement to end TB.
The Deadliest Infectious Disease
TB is an infectious disease, passed from person to person. It spreads through the air when people who are already sick cough, sneeze, talk, or spit—which can result in infection. It’s necessary, but not sufficient, to develop into TB disease. Moreover, diabetes, a weakened immune system, and malnutrition can increase someone’s risk of contracting TB disease.
“Being a contagious disease transmitted by air, anyone can get tuberculosis, even after years of being exposed to the bacteria,” Dr. Leonid Lecca, executive director of Socios En Salud, as PIH is known in Peru, said. “There are conditions of the person—age, immune system, presence of diseases—socioeconomic conditions—overcrowding, poverty—and conditions of health services—limited access—that make certain populations more vulnerable to TB.”
When bacteria from the TB infection spreads, it steadily affects different organs in the body, usually starting with the lungs. Common symptoms include a prolonged cough, chest pain, weakness, fatigue, and fever. However, these symptoms may be mild for many months, or some patients may not experience any outward indication of the infection at all, making it easy to spread TB without knowing you have it.
Some people may even have TB infection, be asymptomatic, and potentially days or years later, experience active TB disease. In both cases, however, treatment is available. With TB infection, patients can take preventative therapy to avoid ever getting the active disease—and avoid transmitting it to others. If TB disease develops, there are proven treatment methods that can cure patients, and also help them avoid spreading the disease.
People who develop active disease often experience progressive destruction of the lungs, which, over time, can cause death due to respiratory failure—when people can’t get enough oxygen or eliminate enough CO2—or due to shock or suffocation secondary to blood loss. Even before death, the experience of coughing up blood can be extremely distressing.
Preventing the Spread of TB
Globally, around 30% of TB cases are never diagnosed or treated. However, when people with TB do access treatment, it is highly successful, curing upwards of 80% of those who receive it. And while treatment is often seen as the most important tool, an effective TB response usually starts before a patient is sick.
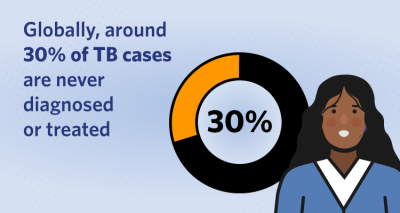
Graphic by Mariel Alvarado / PIH
The best way to prevent TB is to redress the inequalities that increase a person’s risk in the first place—working to ensure people have adequate food, preventing overcrowding, and ensuring adequate ventilation and medical care in settings like dormitories, factories, mines, prisons, and jails where TB can spread rapidly.
“We’ve known what successful interventions for TB look like from experiences in the U.S. and elsewhere since the mid-20th century, including sustained support for public health services, improved living conditions and nutrition, and policies that facilitate universal access to compassionate, respectful health care,” Carole Mitnick, PIH senior research associate and Harvard Medical School professor of global health & social medicine, said.
Seeking medical attention, getting tested for TB if you are experiencing any symptoms—particularly if you are at an increased risk or have come in contact with someone infected by TB—and prompt treatment, whether for active TB disease or through TB Preventative Therapy, can help stop the disease from spreading and improve your chance of recovery.
“Early detection and timely and correct treatment are useful tools that reduce TB transmission in the community,” said Lecca.
Treatment is one of the strongest forms of prevention, not only saving lives but also interrupting the transmission of disease. Someone who is cured of TB can’t spread it to those around them.
Treating TB takes time and diligence, even in the early stages of the disease, making treatment support important to success. Normally, when you think of bacterial diseases that require treatment—strep throat, ear or sinus infections—you get a course of one single antibiotic from your care provider, and everything clears up relatively quickly, generally within days or a week. For TB, however, a cocktail of multiple antibiotics must be taken over four to six months.
Additionally, TB bacteria have been shown to mutate and become resistant to drugs, resulting in the deadlier and more difficult-to-treat multidrug-resistant TB (MDR-TB) or extensively drug-resistant tuberculosis (XDR-TB). PIH was instrumental in showing that these forms of TB are treatable and in finding better, safer, and shorter combinations of drugs to do so.
“With new innovations in TB care led by PIH, the options and prognosis for people suffering from this form of TB are vastly improved,” said Mitnick. “Nearly all people with simpler forms of MDR-TB can be treated in 9 months or less. The treatment is much shorter, compared to 18-24 months, and more effective than the treatments used in the very recent past.”
The Burden of Disease
While TB occurs everywhere, 80% of cases and deaths are in low- and middle-income countries. Though improved treatments and tools, such as PCR testing with GeneXpert, can make a difference today, they are out of reach of many in countries where TB is most prevalent due to continued high prices, intellectual property models that favor originators and investors, cash-strapped governments forced to pay debts rather than support investment in health care, and low global prioritization of TB. Until these conditions change or improve, TB will continue to be a public health threat, causing grief and suffering where treatment and survival are possible.
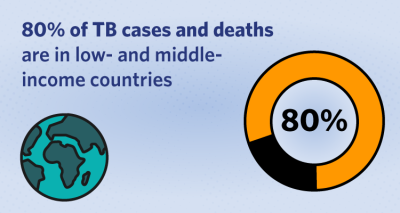
Graphic by Mariel Alvarado / PIH
Recent executive orders to halt foreign aid programs will exacerbate these challenges. The U.S. government is the largest bilateral TB donor, investing more than $4.7 billion to combat TB globally since 2000 through USAID. The interruption of this support endangers lives from Kansas to Kazakhstan and could set progress back by years.
Millions of people should not be dying of a preventable and curable disease. For years, TB has struggled to get global attention, resources, and funding despite ambitious targets like the UN’s goal to end TB by 2030. While we see progress being made at PIH sites around the world and through global partnerships like the endTB clinical trials, there is still much more work to be done.
“Since we know how to search for, treat, and prevent TB, the failure to do so is particularly outrageous,” said Mitnick. “The 70 cases diagnosed in recent months in Kansas, among the nearly 11 million occurring globally in the last year, could have been averted.”
Originally published on pih.org
