There are nearly 1 million new cancer cases and more than 500,000 cancer-related deaths in Africa per year, and these totals are projected to double by 2040. Training the next generation of health leaders to counter this rise is of critical importance. Increasingly, we see a need for cancer education that explores both the prevention measures and social determinants of this highly treatable, but highly prevalent, disease. In recognition of World Cancer Day, we spoke to the University of Global Health Equity’s founding Dean, Prof. Abebe Bekele, to spotlight his holistic approach to cancer education.
Q. This is the first academic year for students in UGHE’s new medical program. Those students arrived on campus last summer and will study for more than six years. They’ll have significant interaction with Butaro District Hospital, the Partners In Health-supported facility across the valley. What have the medical students seen of the hospital so far, and particularly its Cancer Center of Excellence?
UGHE’s MBBS program has an integrated curriculum. Students don’t spend the first two years just in the classroom or the lab—they get exposure to clinics, health centers and health posts, right from the start. We call this progressive clinical immersion. Already, our students have visited the hospital twice, met the medical doctors, visited the health centers and spent time in the community. In January, they will start their basic sciences training, which consists of all the basic sciences in an integrated manner with clinical care. Students will spend time in the hospital, with patients and learning vital communication skills, alongside cancer diagnosis and treatment.
Q: How will students’ involvement with the hospital grow in years to come, through UGHE’s focus on progressive immersion within the curriculum?
Progressive clinical immersion is vital as it serves to blend and balance basic medical and clinical sciences. The first two years are focused mainly on basic medical sciences. That focus decreases as they progress, in a way that’s directly proportional to an increased focus on clinical sciences, with year three as the intersection. Why do we do this? It’s tied to the competencies: What kind of doctors are we trying to train, and what do we need them to do after graduation? These students will go on to diagnose and treat patients, conduct and understand research, serve as health system leaders, advocates of equity, and scholars. So we need to reverse-engineer the curriculum; defining the competencies first, then designing the curriculum, in a way that’s tailored to equip the students with the competencies.

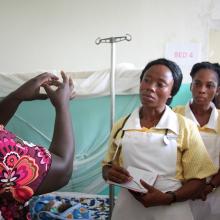
Prof. Abebe Bekele, dean of the University of Global Health Equity in northern Rwanda, said prevention should be the starting point for slowing the rise of cancer cases across Africa.
Courtesy of University of Global Health Equity
Q. How does the integration of humanities in the curriculum contribute to students’ holistic approach to health delivery?
Humanities directly ties to clinical care within the cancer center. Our students learn about African history, the social determinants of health, political economy, gender and justice, and examples that relate to health, such as the identification of lymphoma in Uganda, Ebola, and the health impacts of the rubber industry in the Democratic Republic of the Congo. These examples directly tie to cancer care, looking first at the reasons behind the resurgence of cancer in Africa as a starting point.
Q: What makes the study of cancer, and cancer care, different from other medical areas of focus?
Data shows that cancer is on the rise in Africa. We need to prepare our doctors to first appropriately diagnose the diseases, then promptly refer these cases to proper therapy, and later, as they mature in their careers, consider specializing in cancer care to cater to these growing numbers. We should be looking at prevention as the starting point. Breast and cervical cancer are the two most common cancers affecting our population. Cervical cancer is preventable with appropriate vaccination, and both are treatable if diagnosed early.
Q: What are some examples of how UGHE students will study cancer, in the classroom or outside of it?
When our students enter their clinical years, they’ll spend significant time in the cancer ward: learning and contributing to quality improvement, data collection and research. In terms of research, our MGHD students complete research papers about cancer in the cancer hospital. This emphasis on research also is strongly supported by our faculty; the basic sciences team is developing a proposal in breast and colon cancer, something we hope will help students become more engaged in the subject.
Q: The WHO reports that cancer cases numbers could double by 2040 without strong counter-measures. How can UGHE play a role in addressing, and preparing for, Africa’s growing cancer crisis?
The most common cancers in Africa—breast and cervical—are preventable, or, if not, early diagnosis gives us greater success in treating them. All of us have a role to play here: as physicians, nurses, public health experts, advocates, governments, policy makers and others. If we collaborate and contribute to the prevention of those cancers, we can rapidly reduce the number of cases we see. Advocacy is important. UGHE trains its students to become experts in the diagnosis of cancers, as well as advocates and drivers of social mobilization and policy support for the government.
We also teach our students about equity in everything we do; it is the centrepiece of academics at UGHE. Women have better health-seeking behaviour but they face enormous barriers to accessing care. They are restricted by finances, transport, access to hospitals, cultural taboos, responsibilities at home, gender-based biases and other factors.
Things are stuck at the moment, but not because of lack of awareness—we already know about and understand the mounting incidence of cancer in the continent. It is about who is going to take the bold step to address it.
We have not yet declared cancers as an emerging public health problem in the region. Now is the time to focus on cancer, now is the time to take action.