Conjoined Twin Sisters Successfully Separated in Haiti
Rebecca E. Rollins / Partners In Health
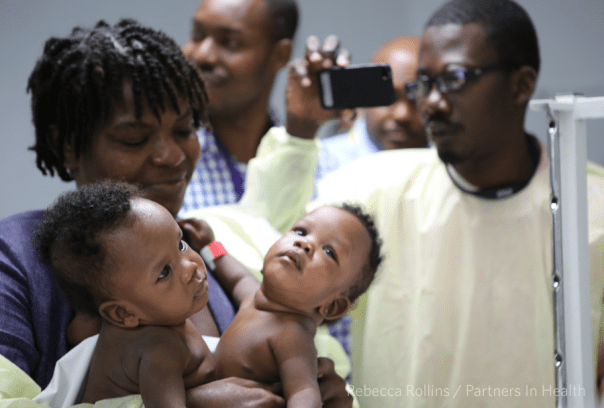
Manoucheca Ketan holds her conjoined twin daughters before their separation at University Hospital in Mirebalais, Haiti, on Friday, May 22.
Manoucheca Ketan lay on an exam table as her doctor spread warm goo over her expanded belly and methodically traced an ultrasound wand back and forth. Black-and-white images of different shapes and sizes appeared on a nearby screen. They looked foreign to her, but clearly meant something to the doctor.
“Pwoblem! Pwoblem! Pwoblem!” he said in Haitian Creole.
Ketan, 35, asked what was wrong. Still staring at the screen, the doctor said he saw three heads and that, from the way the babies were positioned, he thought two of the babies’ bodies were connected.
Ketan was shocked. She’d only wanted one pregnancy, but her husband, David Bernal, wanted more than one child. Apparently both their wishes would come true. Yet the challenges were daunting: How would they afford food, clothing, diapers, and schooling for three children? Where would they find space for everyone? And what if the doctor were right—what if she had conjoined twins?
Her worries only increased. As her pregnancy advanced, Ketan and her private doctor in Port-au-Prince planned for the delivery. He proposed taking the triplets by cesarean section at 6 months. Because the babies would be significantly premature, he said post-partum care would be $1,000 a day for each child. Factoring in the cost of her delivery, he estimated her bill at $100,000.
Before Ketan sank into despair, her younger brother happened to suggest she visit Mirebalais, a town in Haiti’s Central Plateau. He’d heard that patients receive free care at University Hospital (HUM), a state-of-the-art facility that Partners In Health (PIH) and Zanmi Lasante (ZL)—its sister organization in Haiti—had opened there in partnership with the Haitian Ministry of Health in 2013.
Ketan was in her sixth month when she arrived at HUM last August to meet with Dr. Christophe Milien, the hospital’s director of obstetrics and gynecology and advisor to the medical director. After an hour-long ultrasound exam, Milien confirmed Ketan was carrying triplets and that two were conjoined at the abdomen.
“The guarantee I can give you,” Milien told Ketan, “is that we’re going to look for help for you so that we can keep these babies alive.”
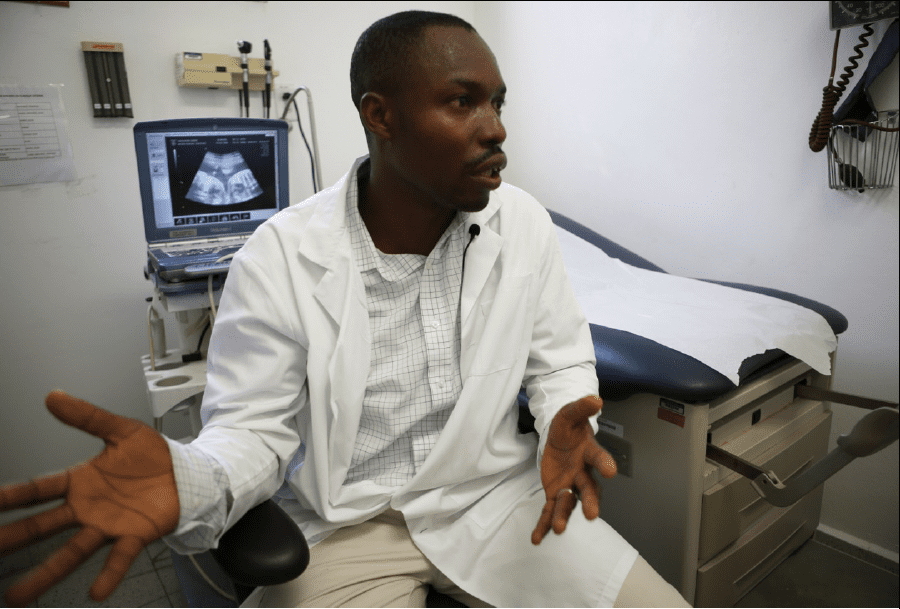
Dr. Christophe Milien, HUM’s director of obstetrics and gynecology, discusses the ultrasound in which he confirmed Manoucheca Ketan was pregnant with triplets, with two infants conjoined at the abdomen.
One in a million
Milien was true to his word, but it was no small task to which he’d committed the HUM team. Conjoined twins are a rare phenomenon, occurring once in every 200,000 live births, according to a report by the University of Maryland Medical Center. Ketan’s pregnancy was even rarer. Conjoined twins within a triplet pregnancy occur in less than one in a million deliveries, according to an article in Case Reports in Obstetrics and Gynecology.
Their outlook wasn’t good. Just over a third of conjoined twins survive only one day, according to the same University of Maryland Medical Center report. And their overall survival rate is between 5 and 25 percent. But for some reason, female siblings survive more often than males. About 70 percent of all living conjoined twins are girls.
Identical twins form when a single embryo splits in half during the first few weeks following conception. Most scientists agree that conjoined twins form when the division of this single egg stops before the process is complete. The partially split egg continues to develop into a conjoined fetus.
Dozens of variations of conjoined twins exist. About 40 percent of all cases are thoracopagus twins, who are connected at the upper portion of the torso and usually share a heart. Omphalopagus twins occur a third of the time and share a liver, gastrointestinal tract, or genitals. Craniophagus twins share a head and are the rarest type, occurring only 2 percent of the time.
Ketan’s twins were omphalopagus and CT scans revealed they shared a liver, but no major vasculature—a fact that made their separation more viable.
Overall, the HUM team’s challenge seemed daunting. They had to prolong Ketan’s pregnancy as much as possible to ensure the best outcome for the triplets, monitor the twins carefully to avoid infections and ensure weight gains, and assemble a team of experts to perform the separation procedure—the first of its kind in Haiti.

A 36-week milestone
Milien didn’t know how any of this would work out in August when he promised Ketan she was in good hands. He admitted her that day to treat her anemia, then kept her on bed rest. Triplets usually deliver around 30 weeks, or 10 weeks early, so he and HUM staff expected they would be caring for premature infants.
When Ketan reached 25 weeks, Milien thought it would great if she could get to 30. When she reached 30 weeks, he aimed for 32. She was still going strong two weeks later. Finally, at 36 weeks, she felt contractions and the HUM team prepared for her C-section.
The night before the surgery, stress got the best of Ketan as the reality of having triplets, two of them conjoined, sank in. She worried about how she would care for and get around with the babies. She worried about the twins’ eventual separation surgery. And, possibly the most difficult part for a new mother, she worried about whether she would love her conjoined twins.
“I didn’t know how I would feel,” Ketan says. “That was a very, very difficult time.”
Milien and other HUM staff reassured Ketan. Discussing what would happen from the moment the children were born up through the separation procedure, they managed to relieve a great deal of her stress.
On November 24, a crowd of HUM staff gathered outside the operating room. Milien and Chief Nursing Officer Marc Julmisse led a team that had practiced for Ketan’s C-section hours of simulation training. Staff stood at attention, half of them wearing red, the other half in blue according to which baby’s team they belonged. An air ambulance perched on a landing strip alongside the hospital, ready to whisk the babies away to the closest facility with a functioning intensive care unit should they need specialty care.
It all followed Julmisse’s motto: “Plan for the worst; pray for the best.”
Apparently those prayers were answered. Milien delivered Tamar. Then he delicately reached in to find the twins, Michelle and Marian—in exactly the same position his most recent ultrasound indicated they would be. All three screamed their greeting into the world; there was no need for a ventilator.
Applause erupted from behind the observation windows, where HUM’s medical director Dr. Maxi Raymonville and Deputy Medical Director Dr. Pierre Marie Cherenfant stood among a crowd of other HUM cheerleaders.
Settling in to a new life

Ketan cradles the sleeping twins on her lap, while Tamar rests on her grandmother’s lap.
Within days, Ketan was on her feet and went to visit Tamar, but she couldn’t bring herself to Michelle and Marian’s bedside. “Initially it was really, really hard to see them,” she says. Racked by guilt and worry, she cried for the first couple of days before she was ready, at Milien’s encouragement, to visit them.
Julmisse and her staff had set the triplets up in their own room following the surgery so they could receive specialized care and privacy. Nurses kept the twins’ materials and medicine color-coded throughout their stay to avoid confusion. They taught Ketan how to feed, hold, and carry her unique twins. Slowly her bond with them grew.
Tamar—who inherited her mother’s easy, broad smile—was the first to come home, which was now a five-minute walk down the road from HUM. PIH/ZL staff had helped Ketan and her husband find an apartment nearby, making follow-up appointments at the hospital and home visits from nursing staff all the easier. Marian and Michelle—who were identical and held hands and tugged on each other’s clothing—followed several weeks later. Ketan’s mother moved in to help out.
On a late afternoon in early May, Ketan sat in her dark living room with the twins settled on her lap facing one another. They sucked each other’s hands while their mother fanned them with a piece of paper. The heat was especially brutal and wasn’t abating with the setting sun. When Julmisse—who was calling on them for a home visit—switched their hands to their own mouths, they swiftly reverted back to their preferred position. Clearly sister’s hand tasted better.
Tamar lay in a neighboring crib and underwent physical therapy with a visiting nurse. Bigger and stronger than her sisters, she was learning to sit on her own and instantly smiled when the nurse held her up to a standing position.
The twins were steadily gaining weight, going through a container of formula each day, in anticipation of their separation at the end of the month when they would be six-months-old. As with other babies who can’t lie on their backs, their heads hadn’t rounded out and looked narrower than their sister’s. Ketan did her best to ensure the twins weren’t falling far behind, despite their limited mobility.
But going outside was tricky. Ketan was reluctant to expose her twins to others’ stares. People frequently asked her how the twins “got stuck together.” She tried to explain, but often came up short and wished more people understood and accepted her daughters as she had.
More than a village
Shortly after Milien diagnosed the twins as conjoined, the HUM team began planning for their eventual separation. One of the first calls was to Dr. Henri Ford, vice president and chief of surgery at Children’s Hospital Los Angeles, who was on HUM’s advisory board and a friend of PIH Co-Founder Dr. Paul Farmer. Ford began assembling a team of experts, including Dr. James Stein, associate chief of surgery at Children’s Hospital Los Angeles, who would travel to Mirebalais for the groundbreaking procedure. Nearly every week he called the HUM team to hammer out details of the surgery, and he visited monthly to check on the twins’ progress.
“It takes more than a village,” said Ford. “It takes probably a village and a city to effectively plan the separation of conjoined twins because you’re thinking in two for every single thing.”
Meanwhile, Dr. Michelle Morse, deputy chief medical officer for Haiti, coordinated the complex operation from her base in Mirebalais. Dr. Romain Jean Louis, the hospital’s director of pediatrics, checked on the triplets weekly. And Julmisse meticulously tracked down materials and equipment, brought her team up to speed, and recruited nurses from U.S. hospitals to help fill the ranks. Extra staff were required for the days of round-the-clock, intensive care that the twins would need following separation.
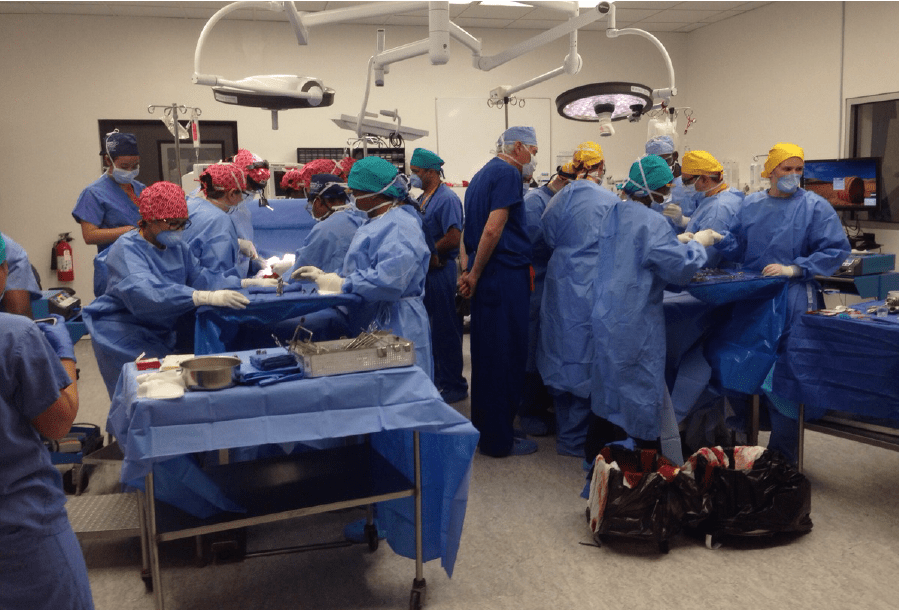
The national and international teams came together in Mirebalais on Thursday, May 21, to run through simulations. Everyone was divided into color-coded teams—red for Marian, yellow for Michelle.
“If we are satisfied that everyone is ready on May 21, then our plan is going to be to proceed with surgery the next day,” said Ford. “If not, we will take our time until everybody is fully aware and fully comfortable with their role before we do the operation.
“It’s a very collaborative process; everybody has a voice,” he added. “We are all motivated by the same purpose: We want to make sure we optimize the chance for these children to go through this separation safely and have meaningful, productive lives without any complication.”
Although nerves were on edge until late in the evening, the Thursday simulation finished strong. Friday, everyone decided, would be the day.
Separate, but together, at last
On the morning of Friday, May 22, Ketan tightly hugged her twins in a staging room near the operating room. Her husband floated in the background, his cell phone recording the moment. Both parents planted kisses on their daughters’ cheeks before Marie Paul, HUM’s chief nurse of surgery, wrapped a blanket around the twins’ waists—the site where they would soon be separated—and marched them to the operating room.
Four hands, arms, legs, and feet wriggled and intertwined as the twins lay on an operating table surrounded by a couple dozen doctors and nurses. With great care and coordination, the team calmed the children, prepared them, and put them under for what would be a seven-hour procedure including pre- and post-surgery care.
The first incision was made at 1:14 p.m. Just over an hour later, Michelle and Marian had been separated. There was a quick cheer before the entire team split into two groups to separately attend to the infants.
The only major complication ended up being a miracle of sorts. Michelle had a fist-sized ovarian cyst that, had it not been discovered, would have caused problems in the near future. Milien, who stood like a sentinel at the foot of the surgical table, immediately scrubbed in, drained, and biopsied the cyst. Fortunately, the benign growth had stretched the girls’ skin so much that enough remained to close their wounds. Surgeons finished the procedure by creating a new belly button for each baby.
As he had throughout the surgery, Milien visited the girls’ parents to tell them the good news. Ketan, who hadn’t eaten all day, breathed a sigh of relief—the worst was over.
By early evening, Michelle and Marian laid in separate cribs in HUM’s intensive care unit, which had recenty opened. Tubes crisscrossed their bodies, but they were stable and sleeping peacefully. Within 48 hours, they were breathing on their own. Within 72 hours, they’d already had their first bottles. And nurses noticed one curious thing: Michelle would calm down whenever they rubbed the side of her face where Marian used to be.
Ketan couldn’t stop smiling as she gazed at her twins. It felt safe now to talk about the future, her daughters’ future, apart and together. She decided she wasn’t going to be the type of mother who told her children what to do, but would help guide and direct them. “I would love to see them develop their full potentials in whatever path they choose,” she says.

Photo by Diane Sherman for Partners In Health
(Left to right) Michelle, Marian, and Tamar Bernal rest in the same crib days after the twins’ separation.



