Cancer and Chronic Diseases
Dr. Cyprien Shyirambere, oncology program director for Partners In Health in Rwanda, records medical information after seeing patients for follow-up visits at PIH-supported Butaro District Hospital.(Photo by Cecille Joan Avila/PIH)
Diseases more commonly associated with wealthy countries, such as cancer, heart disease, and diabetes, are significantly on the rise in poor countries.
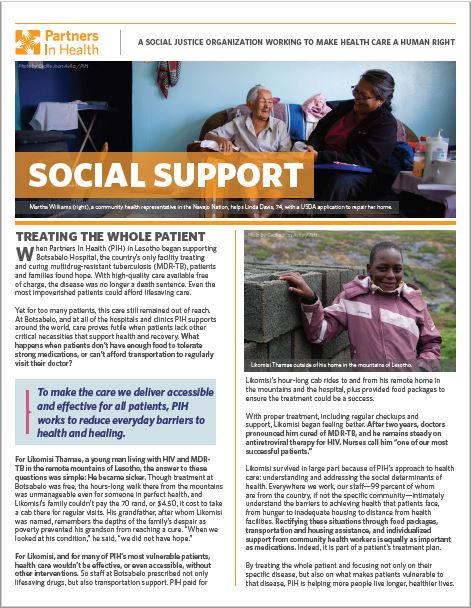
Partners In Health rejects the idea that providing cancer care or treatment for mental health conditions, for example, are too challenging in resource-poor settings. Our work has shown that treating the burden of disease based on patient needs, whatever they may be, can and should be made accessible everywhere.
Partners In Health works to ensure that everyone living with a non-communicable disease (NCD) receives health care by helping governments incorporate NCD programs into their public health systems and by building, advocating for, and implementing strategies that involve local, regional, and national partners.
The World Health Organization estimates that each year 41 million people die from NCDs, with 15 million of these people between the ages of 30 and 69 years. They estimate that over 85% of these “premature” deaths occur in low- and middle-income countries. Although roughly 70 percent of cancer deaths occur in low- and middle-income countries, they receive only five percent of global cancer resources.
Identifying and treating NCDs requires a dedicated global effort. If nothing changes, it is estimated that by 2025, NCDs will cost poor countries $7 trillion in lost earnings of people who suffer these diseases, keeping millions of people trapped in poverty. Mental health challenges represent another devastating burden, with depression poised to become the leading cause of disability worldwide by 2030.
As part of the broader PIH programs to address NCDs, PIH Canada is committed to supporting and advancing cancer care in the countries where we work. By meeting this extraordinary burden with proven methodologies in early detection, prevention, and treatment, we see an entry point for oncology program design that can strengthen entire health systems.
Cancer plagues people in all the countries we work, but we provide the most extensive care in Rwanda and Haiti. In Rwanda, this involves supporting the Butaro Cancer Center of Excellence (BCCoE). Built in 2012, the BCCoE is Rwanda’s first facility dedicated to cancer care and now provides high-quality cancer care to 1,500 patients a year and serves as a national cancer referral center as we support the Ministry of Health’s effort to develop cancer centers in other referral hospitals around the country.
The University Hospital of Mirebalais, Haiti, serves as the country’s finest tertiary care facility. The hospital was opened in 2013 and today provides direct and comprehensive cancer care to a catchment area of 1.2 million patients, as well as training and guidance to clinicians across 11 other PIH-supported facilities in the country.
The PIH cross-site mental health program seeks to establish safe, effective, culturally sound mental health services as a fundamental piece of care continuum, using principles of decentralization, task-sharing and integrated care as a program building blocks. Merging mental health into the stream of primary care enables us not only to address co-morbidities but also to better connect service delivery with existing platforms for training, monitoring and evaluation, quality improvement, and research.
Inshuti Mu Buzima, as Partners In Health is known in Rwanda, and Zipline partnered to find an innovative solution to delivering lifesaving cancer medication through drones to oncology patients during the COVID-19 pandemic response.
Our Impact

More than 17,900 patients with non-communicable diseases in regular care.
More than 3,200 patients receive cancer care every year.
Patient Care: A moral mission, in a medical context
Patients are not only PIH’s main source of inspiration; they’re also our main source of information. We rely on their experiences to inform how we infuse health systems with the staff, stuff, space, and systems required to deliver high-quality care. Download the free resource to learn more about PIH’s patient-centered care.
MAKE A DONATION TODAY TO SUPPORT CANCER AND CHRONIC DISEASE SERVICES AND STRENGTHEN HEALTH SYSTEMS AROUND THE WORLD.
Related stories

Patient Living with Diabetes Regains Health and Hope
In Mexico, PIH provides chronic care for hundreds of patients each year Posted on Dec 21, 2023 Carlos Vázquez is originally from Pequeñez, Chiapas. At 67 years old, he continues to work on his farm, where he grows coffee, corn, and beans a few meters from his home. He has

“All Possible Care”: The Strides and Limits of Emergency Care in Sierra Leone
Luck and a team of determined clinicians saved James Fatoma’s life Posted on Aug 8, 2022 James Fatoma moved to Kono District, Sierra Leone, when he was in high school—and from his teens through his early 30s, had only been to the doctor once. That checkup was five or six

Research: Improving Breast Cancer Outcomes for Patients in Haiti
Earlier detection, diagnosis, and treatment can save lives Posted on Nov 4, 2021 In Haiti, breast cancer is the most common form of the disease among women, as it is worldwide. But there’s a key difference: a higher percentage of women will die from breast cancer in the Caribbean nation