New App Widens Access to Women’s Cancer Screening

The mUzima app will streamline patient data, improve care delivery
Posted on March 9, 2023
On a sunny Wednesday morning, women of varying ages wait outside of a room tucked in a corner of Butaro Health Center.
Each woman is here for a breast cancer or cervical cancer screening.
Inside the room—dedicated for screening for women’s cancers—is a nurse named Raissa Umutesi, who has worked at the health centre for 15 years.
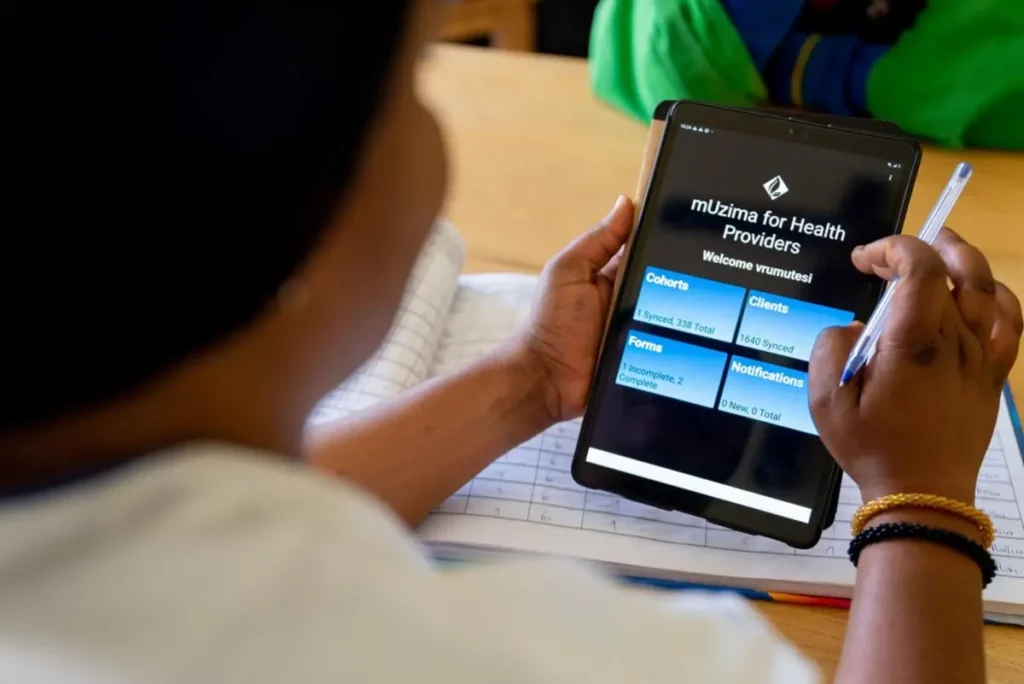
One by one, Umutesi meets with the women and performs breast exams to check for abnormalities or lumps, along with pap smears to examine the cervix. Luckily, none of the patients today have symptoms of breast or cervical cancer—two of the cancers that most often affect women. After each screening, she records the patient information using a tablet.
Just a few years ago, she would have been writing those notes by hand.
Early Detection
Breast and cervical cancer are among the most common forms of cancer affecting women worldwide, making screening and early detection—including for women who appear healthy—critical.
“Breast and cervical cancer can be cured when detected early,” says Umutesi.
Across Rwanda, women can access free cancer screenings from Partners In Health, known locally as Inshuti Mu Buzima, in partnership with other NGOs and the Ministry of Health. These screenings are offered as part of Inshuti Mu Buzima’s Women’s Cancer Early Detection program, a Partners In Health initiative that connects thousands of women with lifesaving treatment. The program typically involves training community health workers and nurses to provide education, screening services, and referral pathways for patients who need further care.
Since the program expanded across five districts in Rwanda in 2018, there has been a significant increase in the number of women seeking cancer screenings. The influx of patients has, however, challenged record-keeping systems—historically, a logbook with hand-written notes about a patient’s personal information, test history and results, and next course of treatment.
For nurses like Umutesi, managing piles of logbooks was overwhelming. But what concerned her most was the risk of losing data and how that would affect a patient’s treatment.
“We receive around 100 women per month,” says Umutesi. “There was a big risk of losing patients’ information. The logbook can easily be lost and extracting information from multiple logbooks is hard.”
In cases where a patient had to be referred to another hospital, their history would often be lost, or key information would be lost in translation, which would hinder the patient’s treatment.
Now, Umutesi and other clinical staff have access to new technology that aims to fix this issue: mUzima.

A New Tool
mUzima is an app allowing health workers to collect and manage patient data on tablets. The app, which can be used offline, securely stores data and is synchronized with a national server on Open Medical Record System (OpenMRS), allowing different hospitals and health centres to access the same data. This ensures that patients with abnormal initial tests can be linked to timely diagnosis and care.
OpenMRS, co-founded by PIH, is tailored for use in developing countries. Today, organizations and governments in 64 countries use this program.
The mUzima app has another important feature: tracking a patient’s appointment history. For instance, if a nurse at a health centre schedules an appointment with a specialist at a referral hospital, they will know if the patient attended their appointment, allowing them to follow up.
“Sometimes a patient faces a problem that prevents them from attending their appointment,” says Umutesi. “We get a notification and call them or contact a community health worker near them to know how we can help.”
Since its launch in 2020, the mUzima app has spread to 16 districts across the country. Partners In Health, in collaboration with the Rwanda Biomedical Center, Clinton Health Access Initiative, and Brigham and Women’s Hospital, has trained over 694 clinicians at 273 health centres and 22 hospitals, enabling the tablet-based tool to be routinely used in the cancer early detection program. And Partners In Health has donated 77 tablets to be used by health care providers at PIH-supported districts.
The impact of mUzima has been remarkable. From July 2020 to December 2022, 167,715 women accessed screening for cervical cancer and 89,449 were screened for breast cancer, according to OpenMRS data.
As Partners In Health continues to accompany Rwanda on the journey to enhance data-driven decision-making to improve health services and outcomes, mUzima is an important tool for managing patient data—and saving lives.
“mUzima application has revolutionized how we keep and manage data about patients,” says Umutesi. “It will benefit the patients a lot.”
Partners In Health continues to work with the Ministry of Health and other partners to expand use of this important application to all health centres in the country.
Originally published on pih.org



